1. Introduction
A recent randomized comparison of liposomal daunorubicin and cytarabine (CPX-351) did not improve response rates or overall survival compared with FLAG-IDA in newly diagnosed acute myeloid leukemia (AML) - although subgroup analyses appeared to show some benefit with CPX-351. The real-world outcomes of these cohorts are unknown. Additionally, there is little data on the relative outcomes of these cohorts in the relapsed or refractory (RR) setting. We aimed to explore the efficacy of CPX-351 and FLAG-IDA with or without venetoclax in newly diagnosed and RR AML outside of clinical trials.
2. Methods
We analyzed 142 patients from the Project ERIS database with newly diagnosed or relapsed or refractory (RR) AML treated with CPX-351 or FLAG-IDA from January 1, 2013 to April 18, 2023 at VCU Massey Comprehensive Cancer Center. We recorded baseline patient-related and disease characteristics, including age, ECOG, Charlson comorbidity index (CCI) scores, molecular profiling and ELN 2022 cytogenetic risk, dates of regimen initiation, and survival. We used the D'Agostino & Pearson method for normality testing and the t-test or Mann-Whitney (as applicable) tests for between-group comparisons. Categorical comparisons used Fischer's exact test. We applied the Bonferroni correction if multiple comparisons were made. The Wilson-Brown method was used for 95% confidence intervals. We analyzed survival by the Kaplan-Meier method with significance determined by the log-rank test. The event for calculating the overall survival (OS) was the date of death. Patients were otherwise censored at the date of last contact.
3. Results
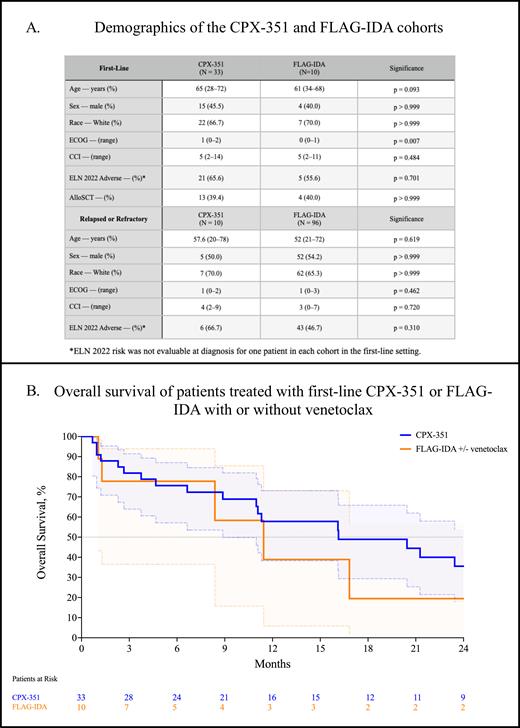
First, we analyzed 43 (30.3%) patients with newly diagnosed AML fit for intensive chemotherapy: 33 (76.7%) received CPX-351 and 10 (23.3%) received FLAG-IDA. In the FLAG-IDA cohort, three (30.0%) patients received concurrent venetoclax. There were no significant differences in baseline characteristics, including age, sex, race, or CCI scores, shown in Table A. However, patients in the CPX-351 cohort had significantly worse ECOG performance status compared with the FLAG-IDA cohort (median, 1 vs 0, p = 0.007). There were no significant differences in the proportion of patients that had ELN 2022 adverse risk cytogenetics between the CPX-351 and FLAG-IDA cohorts (65.6% vs 55.6%, p = 0.701). The composite complete response rate (CRc; CR + CRi + CRh) was 53.6% (95% CI: 35.8-70.5) in the CPX-351 cohort and 62.5% (95% CI: 30.6-86.3) for FLAG-IDA (p = 0.709). The rate of MRD negativity was 33.3% for CPX-351 (95% CI: 5.9-70.0) and 50.0% (95% CI: 2.6-97.4) for FLAG-IDA. A similar proportion of patients proceeded to allogeneic stem cell transplant (alloSCT; 39.4% vs 40.0%, p > 0.999). There was no significant difference in the median overall survival in patients treated with CPX-351 or FLAG-IDA (16.1 m. vs 11.4 m., p = 0.129, Figure B).
Next, we analyzed 96 (90.7%) patients that received FLAG-IDA and ten (9.3%) that received CPX-351 for RR AML in any subsequent line; three (2.1%) patients in the overall cohort received either CPX-351 or FLAG-IDA in the first-line setting, then crossed over to the other arm at disease progression. Sixteen (16.7%) patients received venetoclax with FLAG-IDA. There were no significant baseline differences between cohorts, as shown in Table A. The CRc for CPX-351 was 33.3% (95% CI, 5.9-70.0) compared with 47.7% (95% CI, 37.6-58.0, p = 0.681) for FLAG-IDA. The rate of MRD negativity was 50.0% (95% CI, 2.6-97.4) for CPX-351 and 66.7% for FLAG-IDA (95% CI, 39.1-86.2, p > 0.999). There was no significant difference in the median overall survival in patients treated with CPX-351 or FLAG-IDA (12.7 m. vs 14.5 m., p = 0.561).
4. Discussion
There was no significant difference in the rates of CRc, MRD negativity, or overall survival in patients that received CPX-351 or FLAG-IDA with or without venetoclax in the first-line setting or at the time of disease progression. Both approaches appear to be viable in carefully selected cohorts of patients. A comprehensive toxicity analysis and exploratory molecular subgroup analysis are ongoing.
Disclosures
Grant:Prescient Therapeutics: Research Funding. Maher:Sobi (Doptelet): Speakers Bureau; Bristol Myers Squibb: Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal